ORAL SURGERY
Implantology
Implant procedures involve the implantation of artificial tooth roots into the upper or lower jaw. After a recovery period, crowns can be attached to the implants to replace missing teeth.

 What are implants?
What are implants?Implants have been scientifically proven and relied on for decades. Cylindrical or conical in shape, an implant is a threaded screw made of titanium. The outer threads provide primary stability so that the surrounding bone can fuse to the titanium surface over time. The pre-made base for the crown fits exactly and securely into the implant’s internal threads

 What kinds of implants are there?
What kinds of implants are there?Scientists are currently researching possible alternatives to the time-tested titanium implants. There are some promising leads (e.g. zirconium oxide implants and implants coated with organic material), but these either still remain in the experimental stage or have yet to undergo the long-term research that titanium-screw implants have been subjected to for many years. Blade implants are no longer commonly used.

 What are the advantages of implants?
What are the advantages of implants?The key advantages of implants are:
- Neighboring teeth which are free from decay do not need to be crowned.
- Implants can provide stability for dentures in a edentulous jaw.
- In an incomplete row of teeth, implants can serve as anchors for permanent replacement teeth.

Not necessary to alter neighboring teeth
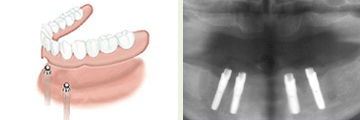
Stability for dentures

Implants on both sides of the upper jaw, dental prostheses
X-ray image of implants
 What is the healing process for implants?
What is the healing process for implants?Depending on the location of the surgery (upper or lower jaw), the quality and stability of the bone tissue, the pressure normally applied to the area, and the type of prosthesis required, the implant may be placed immediately after tooth extraction or at a later time.
Generally, however, the prosthesis is attached to the artificial tooth root after 6 weeks of healing for lower jaw implants or after 3 months for upper jaw implants.
Only the operating surgeon can decide exactly how long the implant should be allowed to heal in each individual case.
 What is the probability that an implant will be successfully
What is the probability that an implant will be successfullyintegrated?
It is approximately 95 %
 How long do dental implants last?
How long do dental implants last?Statistically, 95 % of implants placed by a competent surgeon and well maintained remain intact after 10 years.
 Note Regarding Systemic Diseases
Note Regarding Systemic DiseasesThe risk accompanying dental implantation among patients with systemic diseases must be assessed individually for each case. Well managed diabetes mellitus or osteoporosis does not necessarily preclude implantation.
 What does the treatment cost?
What does the treatment cost?Surgical implantation is considered an elective procedure. The patient should submit the estimated cost to his or her health insurance provider in order to clear up any coverage questions prior to treatment.
 Anatomical Requirements
Anatomical RequirementsThe key requirement for successful implantation is adequate bone tissue at the implant site. The implant must be surrounded by a strong enough layer of bone for long-lasting stability.
The teeth exert necessary pressure on the jaw bone, and when teeth are lost, the jaw naturally begins to atrophy.
The longer a tooth is missing, the greater the extent of the atrophy
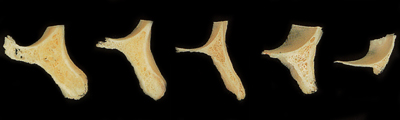
Bone loss after tooth extraction
Advancing atrophy of the upper jaw after tooth loss (cross-section)
In order to prevent complications, the following anatomical structures must be carefully considered:
- The upper jaw bone borders on the maxillary sinus cavities. An implant which is too long could rupture the maxillary sinus, resulting in infection.
- Along the side of the lower jaw runs the inferior alveolar nerve, which transmits sensation from the lower lip and chin. In this area, an implant which is too long could lead to permanent impairment of sensation in the lower lip.
With experience, thorough planning, and accurate diagnosis, in addition to careful implementation of surgical techniques, the surgeon can successfully avoid these problems.

 Planning and Diagnostics
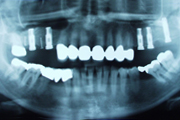
Planning and DiagnosticsAfter a thorough clinical examination, an x-ray image is critical in evaluating the implant bed because the available bone tissue and the relationship between the jaw bone and the neighboring anatomical structures must be assessed.
The orthopantomogram, or “panorex,” is the standard two-dimensional x-ray used in preoperative diagnosis.

Orthopantomogram (OPG)
A much more accurate diagnosis is possible with a three-dimensional, volume-tomographic image from the 3D Accuitomo. This type of x-ray additionally depicts the third spatial dimension and features extremely high resolution. Very often, volume-tomographic images reveal findings that would not be evident in a two-dimensional “panorex.”
3D Volume Tomography
or extensive procedures, a plaster model can be used to facilitate preoperative planning and the design of a drilling guide. The model indicates to the surgeon exactly where the implants need to be placed.


Drilling guide with titanium cylinders on a plaster model and in the patient’s mouth
Three-dimensional preoperative planning is very helpful for extensive reconstructions. Special computer-aided design software can be used to process the information gained through digital volume tomography, creating a precise drilling guide for planning the prostheses.
 Course of Treatment in Non-Problematic Cases
Course of Treatment in Non-Problematic CasesThe operation can be conducted painlessly under local anesthesia or, on the patient’s request, under general anesthesia.
Heavy swelling is to be expected after the operation. Generally, this will start to quickly subside within three days. Patients should also expect to be out of work during this time. The sutures are removed two weeks after the operation.



1. The gingiva is removed from the lower jaw, exposing the bone
2. The implant bed is prepared by drilling
3. The implant is screwed into place, and the gingiva is stitched up

If bone atrophy is too far advanced at the implant site, a preliminary operation may be required in order to build up sufficient bone matter for a stable and long-lasting implant bed.
Materials commonly used to build up the jaw:
Bone matter from the patient’s own body, often from the mouth or hip
Advantage: The patient’s own bone matter has the best chance of successful integration.
Disadvantage: The patient will have an additional wound at the site where the bone is harvested

Bone transplants harvested from the patient
Organic or inorganic synthetic material.
Advantage: No additional wound from bone harvesting
Disadvantages: Lower chance of successful integration, longer healing time, generally poorer bone quality for the implant bed
Your doctor will help you determine the best possible material for your individual case.
 The Most Common Surgical Procedures
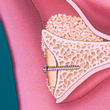
The Most Common Surgical Procedures1. Sinus Lift
This operation is in order when the upper jaw does not have enough bone matter in the vertical plane.

Sinus lift procedure
Source: The Sinus Graft, Ole. T. Jensen, DDS, MS, page 64
The procedure follows these steps:
Diagram A: Atrophied upper jaw; the maxillary sinus is lined with a pink mucous membrane
Diagram B: During the sinus lift, the mucous membrane is raised and the space thus created in the lower part of the sinus cavity is filled in.
Diagram C: The four implants are placed six months later
Diagram D: Three months after that, the implants have healed and the crowns can be attached.
2. Lateral Jaw Expansion with the Patient's Own Bone Matter
A rectangular block of bone is removed from the chin or mandibular angle. This is placed over the area to be built up and affixed with a screw.

Bone matter harvesting for lateral jaw expansion
Source: The Sinus Graft, Ole. T. Jensen, DDS, MS, page 180

Berlin 2010, Dr. med. Dr. med. dent. Herbert Kindermann